An IoT is the internetworking of physical devices, vehicles, buildings, embedded with electronics, software, sensors, actuators, and network connectivity that enables objects to collect and exchange data by controlling remotely across existing network infrastructure, for direct integration of the physical world into computer systems. "Things," in the IoT refers to devices such as heart monitoring implants, automobiles with built-in sensors. These devices collect useful data with the help of various existing technologies. Now a day many textile industries producing a smart textile clothes based on sensors, actuators for functional application. Smart and electronics textiles are widely used in various fields including medical field.
Mobile Health Care is the integration of mobile computing and health monitoring through smart textile clothes for improving communication among patients, physicians. Mobile devices are the important part of our life it can integrate health care more seamlessly to our everyday life with accurate medical information anytime anywhere. Recently developed sensors, low-power IC, and wireless communications have enabled the design of low-cost, lightweight and intelligent biosensor nodes. It the sense, process, communicate integrated into wireless personal or body area networks for mobile health monitoring. In this paper, we present Intelligent Mobile Health Monitoring System with smart textiles, which can provide medical feedback to the patients through mobile devices based on the biomedical and environmental data collected by deployed sensors.
1.Introduction to IoT in intelligent mobile health monitoring system by smart textile
Pervasive computing is the concept that incorporates computation in our working and living environment in such a way so that the interaction between human and computational devices such as mobile devices or computers becomes extremely natural and the user can get multiple types of data in a totally transparent manner. The potential for pervasive computing is evident in almost every aspect of our lives including the hospital, emergency and critical situations, industry, education, or the hostile battlefield. The use of this technology in the field of health and wellness is known as pervasive health care. Mobile computing describes a new class of mobile computing devices which are becoming omnipresent in everyday life. Handhelds, phones and manifold embedded systems make information access easily available for everyone from anywhere at any time. We termed the integration of mobile computing to pervasive healthcare as mobile health care. The goal of mobile health care is to provide health care services to anyone at any time, overcoming the constraints of place, time and character.
In many situations, people have medical issues which are known to them but are unwilling or unable to reliably go to a physician. Obesity, high blood pressure, irregular heartbeat, or diabetes is examples of such common health problems. In these cases, people are usually advised to periodically visit their doctors for routine medical checkups. But if we can provide them with a smarter and more personalised means through which they can get medical feedback, it will save their valuable time, satisfy their desire for personal control over their own health, and lower the cost of long-term medical care.
Various advancements in pervasive computation and communication technologies, coupled with micro and Nanoelectronics have created opportunities for the seamless integration of electronics and flexible sensors. These flexible sensors made of textiles or possessing a clothing-like texture and flexibility result in functionalised textiles commonly referred to as e-textiles or smart textiles. Tao describes smart textiles as a class of smart materials and structures that sense and react to environmental conditions or stimuli. Depending on the degree to which intelligence is imparted into these textiles, they may be passive, active or very smart. Passive textiles only acquire information about the environment active textile reacts to its environment and adapts in different ways, and very smart textiles may be context-aware and adapt their responses based on the context. These three components may be confined to the presence of sensors, actuators and controlling units. For instance, a passive material requires sensors to detect signals. Constituents of an active material may require the coupling of an actuator or a controlling unit with a sensor. Similarly, for very smart textiles, a combination of sensors, actuators, controlling units and a context-aware material that functions as a processing unit may be essential.
Context-aware intelligent materials are formulated by combining conventional textiles with novel materials, mechanics, processing techniques and the chemistry and biology of materials. In biomedical applications for long-term physiological signal monitoring, textiles are the preferred platform for sensors, because they are the most natural materials close to the skin. Traditionally, long-term ambulatory systems that perform biomedical monitoring use adhesives to hold the electrodes or sensors in place against the skin and use a conductive gel to make low impedance electrical contact with the skin. Advancements in analog front-end electronics with very high input impedance and a high common mode rejection ratio (CMRR) have enabled the use of dry electrodes without the need for gels. These dry electrodes, when made on textiles, can be seamlessly integrated into clothing to achieve an intuitive and comfortable alternative to currently available long-term monitoring systems. However, these dry electrodes have been known to have an initial settling time, wherein the contact impedance slowly drops to a value adequate to acquire signals with minimal noise from the environment. One approach to alleviating this problem is to use nanostructured sensors, which have the significantly higher surface area, as compared to planar sensors so that the desirable low contact impedance can be achieved sooner. The review is organized as follows: First, we present the motivations for a textile integrated wearable system from a healthcare perspective for patients who have already been diagnosed with a cardiovascular disease (CVD) Second, we describe the research performed thus far on the use of nanostructured sensors and nanomaterials on textiles for cardiac monitoring. Finally, we present examples of end-to-end system implementations for multi-parameter monitoring through smart devices, namely the e-bra for women and the e-bro for men.
A number of biosensors that monitor vital signs, environmental sensors (temperature, humidity, and light), and a location sensor can all be integrated into a Wearable Wireless Body/Personal Area Network (WBAN/WPAN). This type of networks consisting of inexpensive, lightweight, and miniature sensors can allow long-term, unobtrusive, ambulatory health monitoring with instantaneous feedback to the user about the current health status and real-time or near real-time updates of the user's medical records. Such a system can be used for mobile or computer supervised rehabilitation for various conditions, and even early detection of medical conditions.
As a large amount of medical data is handled by the server, the server will perform mine and analyze the data. With the result of mining, analysis and suggestions and information provided by the specialists in the critical scenarios the server can learn to provide feedback automatically.
2. Sensors in textile
Smart textile (fabric) can be made from materials ranging from traditional cotton, polyester, and nylon, to advanced Kevlar with integrated functionalities. However, in the scope of the present, fabrics with electrical conductivity are of interest. There are two kinds of smart textile (fabric) products that have been developed and studied for health monitoring fabric with textile-based sensor electronics and fabric that envelopes traditional sensor electronics, showed that weaving can be used to incorporate electrically conductive yarn into a fabric to obtain a textile that can be used as a "Wearable Motherboard". It can connect multiple sensors on the body, such as wet gel ECG electrodes, to the signal acquisition electronics. Later research has shown that conductive yarns can be instrumental in the fabrication of textile-based sensors made of fabric or metallic meshes coated with silver or conductive metal cores woven into the fabric.
There are two broad approaches to the fabrication of garments with ECG sensor electrodes in research:
Finished garments through functionalization or integration of finished garments with sensor elements.
This approach involves the integration of finished electrodes into finished garments by simply stitching the electrodes at the appropriate locations on the garment or using deposition techniques to transfer the functional materials at the appropriate locations.
Unfinished garments
The introduction of smart materials during the garment fabrication process. This in Finished approach entails the use of textile fabrication techniques to form woven or nonwoven fabrics with the inclusion of functional materials.
2.1. Incorporation garments
Several flexible and rigid materials have been fabricated and evaluated for use as electrodes. Among resistive electrodes are flexible polydimethylsiloxane (PDMS), CNT array electrodes named ENOBIO, carbon nanotube (CNT)/PDMS Nano composites, flexible polymeric dry electrodes and vertically-aligned metallic nanowires on flexible substrates. Among capacitive electrodes are Ti/TiN electrodes, IrO-coated electrodes, and MEMs spiked electrodes. A comprehensive review of these contact and non-contact dry electrodes has been presented in. Smart textile implementations can be achieved by stitching these electrodes onto finished garments.
2.2. Textiles as electrodes - Unfinished garments
The smallest units of the textile are fibres or filaments. Innumerable combinations of these units can result in many textile materials with varying length, cross-section areas and shapes and surface roughness. The intelligent functionality, conductivity, in this case, can be introduced into textiles at different levels. At the fibre level, a coating can be applied or conductive threads can be added to make a composite textile. Fibres of different types can be arranged at random or in a strictly organized way in yarns or fabrics to form even 3D structures. These structures can be metallized or functionalized to fabricate a conductive textile electrode and other functional surfaces with micro- or Nanorods, or micro- or Nano-coil arrays. Accordingly, there are two strategies followed to make fabrics conductive: Inclusion of thin conductive filaments in the yarns used to make the fabric or coating of the finished fabric with conductive materials by various coating techniques. Mechanical, as well as conductive property.
The inclusion of thin conductive filaments in the yarns used to make the fabric or coating of the finished fabric with conductive materials by various coating techniques. Mechanical, as well as conductive property enhancement, has been documented with the absorption of single-walled carbon nanotubes (SWCNT) in cotton. The latter approach uses deposition and coating techniques, like sputtering, screen printing, electrospinning, and carbonising and evaporation deposition. Conductive coatings on fabric result in higher conductivities, but are less durable, especially through wash cycles. Nanotextiles are formed by the fabrication of nanostructures on textile fabrics or forming Nanoscale filamentous structures on fabric, rather than incorporating nanomaterials into fabrics.
2.3. Nanocomposite inks for conductive traces and connections
Implementations of wearable systems on textile require a cost-effective, as well as scalable way to form interconnects between the various components. One approach to achieving this goal is to have functional inks that can be printed onto a textile to essentially form printed circuit boards on textile. In the case of ECG smart textiles, this involves the formulation of conductive inks or printable capacitive structures on fabric. Polymer thick film (PTF) technologies have been used to form conductive traces and transmission lines on a non-woven fabric in. Alternatively, inks with conductive fillers and polymer binders have been used in the formulation of several inks that are stretchable and resistant to wear and tear. Stretchable conductive inks on textiles have been demonstrated through conductive traces using silver flakes in the polyurethane-based binder by Araki et al..Poly(3,4 ethylene dioxythiophene) : poly(styrene sulfonate) films have been successfully deposited on rubber latex substrates using ink-jet printing. Multi-wall carbon nanotubes (MWCNTs) and polyaniline nanoparticle (PANP) core shell-based nanocomposite conductive inks were synthesized and successfully screen printed on woven cotton by Rai et al. Conductive traces drawn from inks with silver flakes in an acrylic binder have been used to make connections between ECG electrodes and flexible printed circuit boards (PCBs).
3. Examples of systems implementation
Wearable systems for monitoring physiological signals have been reported in many studies. Some of them are in the form of wearable accessories, such as wrist watch for cuffless blood pressure monitoring. Systems can be off-the-shelf electronics with dry electrodes fabricated on FR4 boards that can be embedded/encapsulated in clothing, such as a cap or shirt. The systems either display only or transmit to a remote location through Bluetooth-enabled cellular phone/Zigbee-enabled PC and wireless data transmission or the Internet for remote patient monitoring (RPM). The systems can be microelectronics fabricated on flexible substrates, which are easy to incorporate into the textile. These electronics can accomplish multiple biometric monitoring, such as sweat rate, temperature, ECG, blood oxygen level, etc.
The systems can be microelectronics fabricated on flexible substrates, which are easy to incorporate into the textile. These electronics can accomplish multiple biometric monitoring, such as sweat rate, temperature, ECG, blood oxygen level, etc., along with the wireless transmission. In combination with global positioning technology, they can facilitate medical intervention and augment ubiquitous healthcare. Sensors that are encapsulated, enmeshed or textile-based are predominantly electrical, optical or piezoelectric monitor physiological signals close to the body. Dry electrodes are the most popular type of sensors for biopotential measurement in wearable systems. These electrodes have varying designs, which include fabric made of woven conductive thread, an array of metalized needles, a conductive surface and an Ag/AgCl back electrode (conductive gel free) and capacitively-coupled dry electrodes. They have been shown to acquire biopotential signals. In addition to that, they have been proposed for cardiac, as well as neural stimulation. Optical sensors are mainly off the shelf microelectronics or optical fiber-based sensors. The piezoelectric sensors are off-the-shelf microelectronics, flexible piezoelectric membranes or functionalized piezoelectric yarn. Wireless sensor systems generate large amounts of data that require data management and post processing. Research in database architecture has shown that database organization for the derivation of medical parameters for diagnostics and archiving of diagnostic parameters solves the problem of data volume. In addition to that, data processing through cloud computing and remote access to stored data improves the computing performance. In the following sections, implementations of wearable systems with textile-based nanosensors and state of-the-art wireless communication systems are described.
3.1. E-Bro
The textile platform in this application is an inner vest that can incorporate nano biosensors, such as gold nanowire electrodes or nanostructured textile electrodes and composite piezoelectric films. It can also incorporate an infrared emitter-detection system for plethysmography and temperature sensors. The e-bro system is an implementation of a multichannel wearable wireless textile-based nano-biosensor that monitors ECG and blood pressure.
3.2. System description
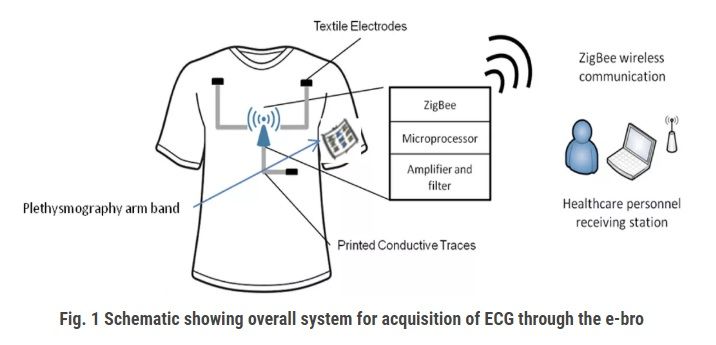 Figure 1 shows the overall system, which consists of four components: firstly, a compression inner vest, referred to as the e-bro, with the textile electrode sensors and the printed connection traces that connect the electrodes to a sensor electronics module (SEM); secondly, a photoplethysmography armband that has near-IR LEDs and photodiodes, which are connected to the SEM through conductive traces printed on the left arm; thirdly, the SEM that consists of an amplifier, filter circuits, a microcontroller and a ZigBee wireless radio; lastly, a software program running on a PC that receives and plots incoming data from the person wearing it.
Figure 1 shows the overall system, which consists of four components: firstly, a compression inner vest, referred to as the e-bro, with the textile electrode sensors and the printed connection traces that connect the electrodes to a sensor electronics module (SEM); secondly, a photoplethysmography armband that has near-IR LEDs and photodiodes, which are connected to the SEM through conductive traces printed on the left arm; thirdly, the SEM that consists of an amplifier, filter circuits, a microcontroller and a ZigBee wireless radio; lastly, a software program running on a PC that receives and plots incoming data from the person wearing it.
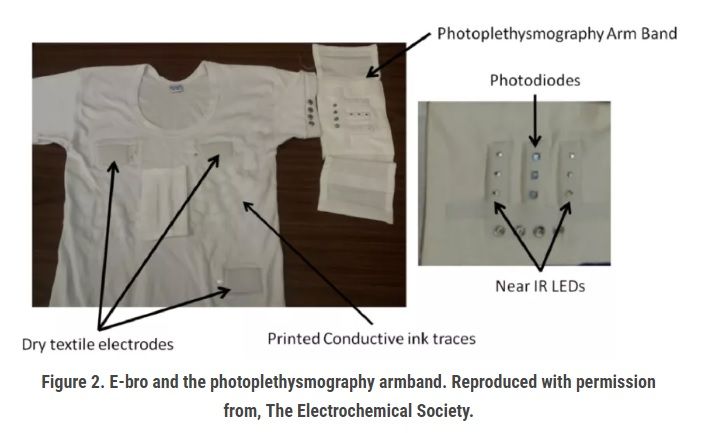
The photoplethysmography armband consists of two arrays of near-IR photodiodes and a central array of three photodiodes. The electrodes and the armband are connected to the SEM through conductive traces, an ink formulation of silver nanoparticle fillers in an elastic acrylic-based binder, printed on the vest, and snap buttons. The conductive traces were made using conductive inks, and screen printing was used, which is textile manufacturing compatible. The armband is removable and simply snaps on to the vest through four snap buttons (Figure 2). The removable SEM and arm band makes the e-bro washable.
3.3. Sensor Electronics Module (SEM)
The amplifier, which is a part of the SEM, consists of four channels: three channels for the bipolar limb leads, Lead I, Lead II and Lead III, and the fourth channel amplifies the potential difference across the photodiode, which detects the reflected IR waves from the brachial artery. The amplifiers used in the SEM had a band pass of 0.2 Hz to 70 Hz and a mid-band gain of 50 dB for the three ECG channels. The gain was increased to 55 dB for the photoplethysmography sensors for a band of 0.2 Hz to 15 Hz. The amplified signals from the amplifier are digitized using the onboard microcontroller for transmission; Figure 3.
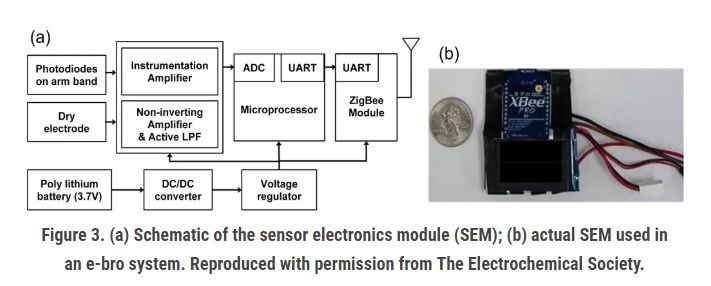
The choice of the Zig-Bee radio module was motivated by two desired functions. Firstly, it has to support data rates higher than 9,600 bps, because four channels of digitized ECG and BP signal have to be transmitted in real time. Secondly, it provides communication ranges as high as possible for applications in sports, military expedition and high-risk work environments, such as firefighters.
3.4. E-Bra
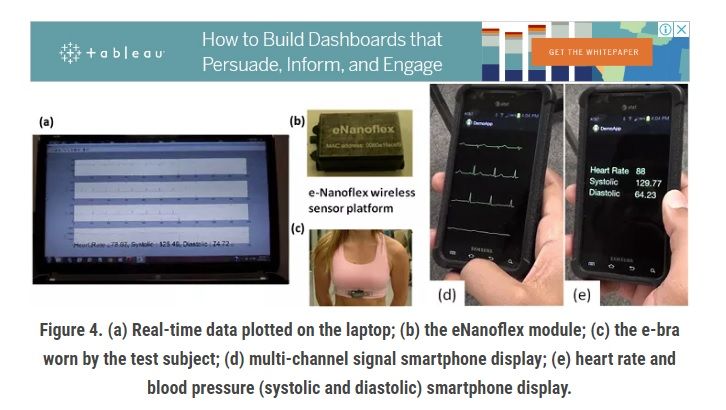
The systems incorporated in the inner vest for men can also be integrated into an inner garment for women, such as a brassiere. The various sensors listed in the previous section can be incorporated in the e-bra and the signals from the sensors brought to the eNanoflex module through printed conductive traces or conductive threads. Figure 4 shows a picture of the e-bra, the eNanoflex module used for data acquisition and wireless transmission and the simple signal display interface that plots the data received from the eNanoflex module.
 3.5. Multichannel data acquired:
3.5. Multichannel data acquired:
The data acquired by the e-bro can be transmitted wirelessly to a PC. The data received by the PC was then filtered using an adaptive filter algorithm to minimize the effect of motion on the ECG signal baseline. The data acquisition and adaptive filter were developed using MATLAB (Mathworks, Natick, MA, USA). However, the same can be achieved on a JAVA platform and can be deployed on a smartphone. Figure 4ad shows the original three ECG signals, Lead I, Lead II and Lead III. It also plots the pulse waveform, the heart rate and the estimated systolic and diastolic blood pressure. The figure shows the eNanoflex module used for data acquisition and wireless transmission. The derived pulse transit time (PTT) values are then used to estimate the systolic and diastolic blood pressure values (Figure 4e) based on the calibration equations previously obtained in. Other sensor systems can be incorporated to develop wearable applications to monitor respiration, temperature, and blood oxygen level. Post processing of ECG can also calculate heart rate variability (HRV), which is a prognostic and diagnostic tool. HRV is described as the sequence formed by concatenating the difference in heart rate between consecutive beats. It is calculated as the inverse of the difference in the intervals between consecutive R-peaks. The R-peak detection algorithm used for the calculation of the RR interval (RRI) was as given in. The autoregressive (AR) power spectrum estimation technique was used to obtain the power spectrum density (PSD) plot of the RRI sequence. The characteristic LF and HF peaks were observed. The figure shows the AR PSD computed from the RRI series for the standing-up case. The figure shows the same for supine ECG. AR PSDs in both figures show a classic shift in the power distribution between LF and HF components with respect to total power.
Thus, these implementations of the e-bro and e-bra systems can be used for the tracking of chronic conditions related to autonomous nervous regulation of cardiac activity. Continuous multiple lead ECG monitoring can be used for the detection of T-wave inversion, which is indicative of a change in ventricular repolarization. Automated post processing of ECG by an algorithm for the detection of T-wave inversion can serve as an alarm system that will trigger a subroutine to initiate the ECG signal relay through a remote server to a doctor's office for diagnosis.
4. System architecture:
IMHMS collects patient's physiological data through the bio-sensors. The data is aggregated in the sensor network and a summary of the collected data is transmitted to a patient's personal computer or cell phone/PDA. These devices forward data to the medical server for analysis. After the data is analyzed, the medical server provides feedback to the patient's personal computer or cell phone/PDA. The patients can take necessary actions depending on the feedback. The IMHMS contains three components.
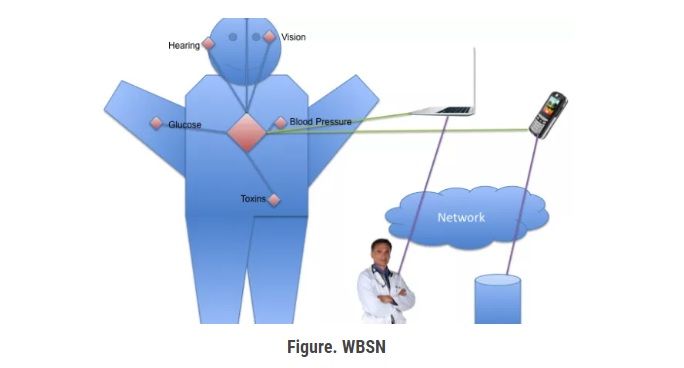
1. Wearable Body Sensor Network [WBSN]
2. Patients Personal Home Server [PPHS]
3. Intelligent Medical Server [IMS].
They are described below.
4.1. Wearable Body Sensor Network [WBSN]
Wearable Body Sensor Network is formed with the wearable or implantable biosensors in patient's body. These sensors collect necessary readings from patient's body. For each organ, there will be a group of sensors which will send their readings to the group leader. The group leaders can communicate with each others. They send the aggregated information to the central controller. The central controller is responsible for transmitting patient's data to the personal computer or cell phone/PDA. Suggested that for wireless communication inside the human body, the tissue medium acts as a channel through which the information is sent as electromagnetic (EM) radio frequency (RF). So in WBSN, information is transmitted as electromagnetic (EM) radio frequency (RF) waves. The central controller of the WBSN communicates with the Patients Personal Home Server [PPHS] using any of the three wireless protocols: Bluetooth, WLAN (802.11) or ZigBee. Bluetooth can be used for short range distances between the central controller and PPHS. WLAN can be used to support more distance between them. Nowadays ZigBee introduces itself as a specialized wireless protocol suitable for pervasive and ubiquitous applications. So ZigBee can be used for the communication too.
4.2. Patient's Personal Home Server [PPHS]
The patient's personal home server can be a personal computer or mobile devices such as cell phone/PDA. We suggest mobile devices because it will be more suitable for the users to use their mobile devices for this purpose. PPHS collects information from the central controller of the WBSN. PPHS sends information to the Intelligent Medical Server [IMS].PPHS contains logics in order to determine whether to send the information to the IMS or not. Personal Computer based PPHS communicates with the IMS using the Internet. Mobile devices based PPHS communicates with the IMS using GPRS / Edge / SMS. The best way to implement IMS is by Web Service or Servlet based architecture. The IMS will act as the service provider and the patients PPHS will act as the service requester. By providing these types of architecture, a large number of heterogeneous environments can be supported with security. So personal computer or cell phone/PDA can be connected easily to a single IMS without any problem.
4.3. Intelligent Medical Server [IMS]
Intelligent Medical Server [IMS] receives data from all the PPHS. It is the backbone of this entire architecture. It is capable of learning patient specific thresholds. It can learn from previous treatment records of a patient. Whenever a doctor or specialist examines a patient, the examination and treatment results are stored in the central database. IMS mines these data by using state-of-the-art data mining techniques such as neural nets, association rules, decision trees depending on the nature and distribution of the data. After processing the information it provides feedback to the PPHS or informs medical authority in critical situations. PPHS displays the feedback to the patients. Medical authority can take necessary measures. The IMS keeps patient specific records. It can infer any trend of diseases for a patient, family even locality. IMS can cope with health variations due to seasonal changes, epidemics etc. IMS is controlled and monitored mainly by specialized physicians. But even a patient can help train IMS by providing information specific to him. After mining the database stored in IMS, important information regarding the general health of the people can be obtained. It can help the authority to decide health policies. Large numbers of patients will be connected to the IMS using their PPHS. So security of the patients is a major issue here. So RFID can be used for this purpose. Radio-frequency identification (RFID) is an automatic identification method, relying on storing and remotely retrieving data using devices called RFID tags or transponders. A RFID tag is an object that can be applied to or incorporated into a product, animal, or person for the purpose of identification using radio waves. Some tags can be read from several meters away and beyond the line of sight of the reader. So security can be provided by providing RFID tags to each patient.
5. Future works and conclusion
The whole system of mobile health care using biosensor network places forward some future works such as finding the most effective mechanism for ensuring security in biosensors considering the severe restrictions of memory and energy, representing the collected data in the most informative manner with minimal storage and user interaction, modeling of data so that the system will not represent all the data but only relevant information thus saving memory. These are the generic works that can be done in future in the sector of mobile health care. For IMHMS our vision is much wider. We think of a system where the patients need not do any actions at all. With the advancement of sensor technologies, it is not far enough when the bio-sensors itself can take necessary actions. A patient needed glucose does not need to take it manually rather the bio-sensors can push the glucose into the patient's body depending on the feedback from the IMS. It seems to be impossible to achieve by everybody. But nothing is impossible. Today we imagine of something and see that it is implemented in the near future. But if we stop imagine and thinking then how impossible can be made possible? This paper demonstrates an intelligent system for mobile health monitoring. Smart sensors offer the promise of significant advances in medical treatment. Networking multiple smart sensors into an application-specific solution to combat disease is a promising approach, which will require research with a different perspective to resolve an array of novel and challenging problems. As wireless networks of sensors are developed for biomedical applications, the knowledge gained from these implementations should be used to facilitate the development of sensor networks for new applications. Expeditious development of implanted smart sensors to remedy medical problems presents clear benefits to individuals as well as society as a whole. There is the obvious benefit to persons with debilitating diseases and their families as these patients gain an enhanced quality of life. Biomedical implants that monitor for cancer will help recovering patients maintain their health. Not only will these individuals personally benefit from their improved health and well-being, but society will also benefit from their increased productivity and societal contributions. Once the technology is refined, medical costs for correcting chronic medical conditions will be reduced. As the world population increases, the demand for such system will only increase. We are implementing the IMHMS to help the individuals as well as the whole humanity. Our goals will be fulfilled.
References:
1. A GOOD AGE: Aging and technology. Tao, X. Smart Fibers, Fabrics and Clothing; Woodhead Publishing: Cambridge, UK, 2001.
2. Zhang, X.; Tao, X. Smart textiles: Passive smart. Textil Asia, June 2001, 45-49; Zhang, X.; Tao, X. Smart textiles: Very smart. Textile Asia, August 2001, 35-37.
3. Van Langenhove, L. Smart Textile
This article has not been edited by Fibre2Fashion staff and is re-published with permission from textilemates.com


_Small.jpg)



